Ketogenic Diet as an Adjuvant Therapy for Inoperable Malignant Brain Tumors
/By Brian Mitchell
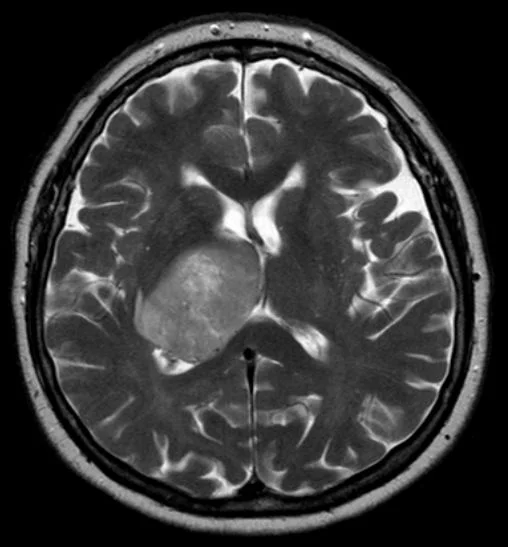
Glioblastoma multiforme (GBM)
Three of the most life-altering words to hear from a physician are inoperable, malignant, and tumor. One of the most common, but insidious, malignant brain tumor diagnoses is Glioblastoma Multiforme (GBM) (American Cancer Society, 2019). With an average survival rate of less than 15 months from diagnosis, GBM is particularly intractable to treatment and quickly spreads to surrounding neuroepithelial tissue, impeding blood supply, which renders chemotherapy even less effective. Gliomas arise from the central nervous system (CNS) glial cells, supporting cells that are intended to maintain the integrity of the nerves by generating myelin, foraging for nutrients, and maintaining the electrolyte balance of the cerebrospinal fluid (Louis et al., 2016). A glioma is typically discovered on an MRI after a patient reports severe headaches, vomiting, difficulty speaking, and potentially a seizure. To make a definitive diagnosis, however, a biopsy is performed by a neurosurgeon to provide a tissue sample of the tumor for analysis (Awad et al., 2017). Traditional comprehensive treatment, with an aim to remove the bulk of the tumor if easily accessible and slow the growth of the tumor with radiation and chemotherapy, is developed collaboratively by the neurologist, oncologist, and neurosurgeon.
Unfortunately, the prognosis is still very poor with only 8-14% of patients diagnosed with GBM being able to overcome the disease (Poff et al., 2019). Cancer researchers are beginning to employ a medical nutrition therapeutic approach to cancer treatment that restricts a tumor’s nutrient supply, thereby slowing the growth of the tumor and extending the patient’s life (Poff et al., 2017). The idea of targeting a tumor’s metabolic limitations is not a new concept, however. In the mid 1920’s, Otto Warburg made a groundbreaking discovery, showing that cancerous tumor cells preferentially metabolize glucose through the glycolysis pathway, even in the presence of oxygen (Warburg, 1956). Glycolysis can occur in both aerobic conditions (respiration) and anaerobic conditions (fermentation), while oxidative phosphorylation (the continuing steps after glycolysis) require oxygen as a terminal electron acceptor in order to produce vast amounts of cellular energy in the form of Adenosine Triphosphate (ATP). A standard cell that has access to oxygen will favor oxidative phosphorylation because the energy payoff is much greater; producing nearly 16 times the amount of energy than glycolysis alone (Warburg, Wind, & Negelein, 1927).
A few explanations for the peculiar behaviors, survival, and growth of cancer cells include the possibility that cancer disrupts the normal functioning of the mitochondria, which is responsible for regulated cell death (apoptosis), and that rapidly growing tumors often outgrow their blood supply, forcing them to adapt to a low oxygen environment (Lopez-Lazaro, 2008). Warburg realized that if he put the tumor cells in an environment without any oxygen, but the cells had an adequate amount of serum glucose, the cell continued to thrive because it would metabolically shift to fermentation to produce energy (Warburg et al., 1927). This discovery, which later became known as the Warburg effect, can be exploited to methodically restrict nutrients that are used to fuel the tumor cell’s functions (Gillies, Robey, & Gatenby, 2008).
During the same time period that Warburg was discovering the metabolic behaviors of tumors, researchers from all over the world were sharing information in an effort to treat epilepsy (Wheless, 2008). In the early 1920’s, a physician from New York Presbyterian Hospital, Dr. Henry Geyelin, studied a child who had been having epileptic seizures for several years. All previous treatments recommended by the prominent neurologists of that age had produced no relief for the young boy, including the use of the phenobarbital and bromide medications. Taking the recommendation of a colleague, Dr. Geyelin instructed the young boy to begin fasting. Within two days, the child’s seizures had ceased entirely, and he remained in remission for several years without the reoccurrence of seizures. Research by Dr. Stanley Cobb and Dr. William G. Lennox revealed that the process of fasting shifts the body’s energy production mechanism from burning glucose to burning fat, which produces acid. This acid decreases the pH of the patient’s blood serum around the second or third day of fasting, correlating with the cessation of seizures (Gano, Patel, & Rho, 2014).
The work of Dr. Rollin Woodyatt built on this concept that fasting produces acids and found that when in the fasted state, the liver produces by-products of fat oxidation known as ketone bodies. Dr. Russell Wilder of the Mayo Clinic later determined that a diet high in fat, but extremely low in carbohydrates, initiated ketogenesis (production of ketone bodies) and induced the same physiological conditions as fasting (Wilder, 1921). Eventually known as the Ketogenic Diet, physicians began prescribing this high fat, moderate protein, and extremely low carbohydrate diet to epileptic patients with overwhelming success (Gano et al., 2014). There were no cognitive or physiological deficits, because all healthy cells in the body can metabolically shift to using ketone bodies instead of glucose for a main source of energy. Normal brain tissue is able to metabolically evolve to use ketone bodies as a fuel source, while cancerous cells depend on glucose in order to perform glycolysis to make energy (Van der Louw et al., 2019).
Making the connection that the ketogenic diet can induce the state of ketosis, and being in active ketosis allows for normal brain cells to continue to survive while concurrently choking off glucose to glioma cells, has allowed physicians and dietitians to implement the ketogenic diet to GBM patients to slow the growth of gliomas by exploiting the Warburg effect (Poff et al., 2017). Data collected during recent studies showed that patients who had elevated levels of blood serum glucose had a much lower chance of survival, which corroborates the tumors reliance on glucose intake (Derr et al., 2009). Furthermore, most patients undergoing treatment to battle GBM are prescribed steroids, which in turn elevates blood glucose (McGirt et al., 2008).
The ketogenic diet contains only 3% of the daily intake from carbohydrates, and therefore does not provide adequate glucose for the tumor to continue to thrive (Gano et al., 2014). A series of mechanisms that are set into motion by ketosis slow the growth of a glioma by reducing blood glucose levels, tempering oxidative stress, regulating inflammation, and strengthening the immune system. This leaves the tumor vulnerable and more susceptible to radiation and chemotherapy. Unlike standard GBM treatment recommendations, the ketogenic diet is unique in that it does not damage all cells in order to target the cancerous tissue, so it can reduce the amount of chemotherapy and radiation necessary (Poff et al., 2016). Radiation therapy done in conjunction with the ketogenic diet has shown to be more successful in shrinking gliomas when compared to performing only radiation (Abdelwahab et al., 2012).
The basic recommendation for a clinical application of the ketogenic diet to target GBM is a 4:1 ratio of fat to protein, with a very small percentage of carbohydrate intake during the course of treatment (Van der Louw et al., 2019). Following the biopsy and removal of the bulk of the tumor (if possible), the patient begins chemoradiation while concurrently starting an exclusively liquid ketogenic diet with 90% of calories coming from fat, 7% from protein, and 3% from carbohydrate intake until the patient achieves ketosis and maintains elevated ketone levels for three days. Once the ketone levels are balanced, solid-food is slowly introduced, and the ratio of fat to protein is modified to 2:1, with the majority of fat being medium-chain triglycerides (MCT), due to its ability to produce higher levels of ketone bodies even with a lower ratio of fat to protein. Because ketone bodies lower the pH of the blood, causing the blood to become slightly acidic, it is very important for regular blood tests to be performed to make sure the patient does not suffer from acidemia (dangerously low blood pH).
An important distinction to make is that the ketogenic diet is not a cure for GBM, but the therapy will potentially increase the survival period for the patient. In one study, a ketogenic diet increased the survival period by nearly 50% (Poff et. al., 2016). In another instance, a patient’s tumors became undetectable on an MRI, but upon ceasing the ketogenic diet the tumors returned and the patient eventually passed away (Maalouf, Rho, & Mattson, 2009). While complete remission of the cancer would be ideal, increased survival time can still be considered an improved outcome.
Some challenges facing this treatment include patients reporting that consuming such a high proportion of their calories from fat was unpalatable at times and was not well tolerated by all of the participants (Van der Louw et al., 2019). Additionally, patients required rigorous encouragement from the dietitians to help solve issues with the diet for it to remain feasible and stay motivated to continue with the nutrition therapy.
Despite these challenges, the use of the ketogenic diet as an adjuvant therapy has been found to be both feasible and safe (Van der Louw et al., 2019). While the prognosis is still very bleak for someone diagnosed with GBM, the benefits of incorporating the ketogenic diet as additional therapy is three-fold. First, because the ketogenic diet does not damage healthy tissue, the metastatic growth cancerous tissue is slowed naturally, diminishing the damage necessary to fight the disease. Second, by slowing or halting the growth of the glioma, the team of doctors has adequate time to consider alternate approaches to combat the tumor. Finally, if the ketogenic diet adds even a few months to the patient’s life, offering them more precious time with family and friends and an extended period to get their affairs in order, then the approach can be considered a success. The fight to find solutions to overcome GBM is still incredibly challenging, but researchers are finally making headway.
References
Abdelwahab, M. G., Fenton, K. E., Preul, M. C., Rho, J. M., Lynch, A., Stafford, P., & Scheck, A. C. (2012). The ketogenic diet is an effective adjuvant to radiation rherapy for the treatment of malignant glioma. PLoS ONE, 7(5), E36197. doi: 10.1371/journal.pone.0036197
American Cancer Society. Cancer Facts & Figures 2019. Atlanta: American Cancer Society; 2019.
Awad, A., Karsy, M., Sanai, N., Spetzler, R., Zhang, Y., Xu, Y., & Mahan, M. A. (2017). Impact of removed tumor volume and location on patient outcome in glioblastoma. Journal of Neuro-Oncology, 135(1), 161-171. doi: 10.1007/s11060-017-2562-1
Derr, R. L., Ye, X., Islas, M. U., Desideri, S., Saudek, C. D., & Grossman, S. A. (2009). Association between hyperglycemia and survival in patients with newly diagnosed glioblastoma. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 27(7), 1082-1086. doi: 10.1200/JCO.2008.19.1098
Gano, L. B., Patel, M., & Rho, J. M. (2014). Ketogenic diets, mitochondria, and neurological diseases. Journal of lipid research, 55(11), 2211–2228. doi:10.1194/jlr.R048975
Gillies, R. J., Robey, I., & Gatenby, R. A. (2008). Causes and consequences of increased glucose metabolism of cancers. Journal of Nuclear Medicine: Official Publication, Society of Nuclear Medicine, 49 Suppl 2(6), 24S-42S. doi: 10.2967/jnumed.107.047258
Lopez-Lazaro, M. (2008). The warburg effect: Why and how do cancer cells activate glycolysis in the presence of oxygen? Anti-Cancer Agents in Medicinal Chemistry, 8(3), 305-312. doi: 10.2174/187152008783961932
Louis, D. N., Perry, A., Reifenberger, G., Deimling, A. V., Figarella-Branger, D., Cavenee, W. K., . . . Ellison, D. W. (2016). The 2016 world health organization classification of tumors of the central nervous system: A summary. Acta Neuropathologica, 131(6), 803-820. doi: 10.1007/s00401-016-1545-1
Maalouf, M., Rho, J. M., & Mattson, M. P. (2009). The neuroprotective properties of calorie restriction, the ketogenic diet, and ketone bodies. Brain Research Reviews,59(2), 293-315. doi: 10.1016/j.brainresrev.2008.09.002
McGirt, M. J., Chaichana, K. L., Gathinji, M., Attenello, F., Than, K., Ruiz, A. J., . . . Quiñones-Hinojosa, A. (2008). Persistent outpatient hyperglycemia is independently associated with decreased survival after primary resection of malignant brain astrocytomas. Neurosurgery, 63(2), 286-291. doi: 10.1227/01.NEU.0000315282.61035.48.
Poff, A., Koutnik, A. P., Egan, K. M., Sahebjam, S., D’agostino, D., & Kumar, N. B. (2019). Targeting the Warburg effect for cancer treatment: Ketogenic diets for management of glioma. Seminars in Cancer Biology, 56, 135-148. doi: 10.1016/j.semcancer.2017.12.011.
Van der Louw, E. J. T. M., Olieman, J. F., Van Den Bemt, P. M. L. A., Bromberg, J. E. C., Oomen-de Hoop, E., Neuteboom, R. F., . . . Vincent, A. J. P. E. (2019). Ketogenic diet treatment as adjuvant to standard treatment of glioblastoma multiforme: A feasibility and safety study. Therapeutic Advances in Medical Oncology, 11, doi: 10.1177/1758835919853958
Warburg, O., Wind F., & Negelein A. (1927). The metabolism of tumors in the body. The Journal of General Physiology 8(6) 519-530. doi: 10.1085/jgp.8.6.519
Warburg, O. (1956). On the origin of cancer cells. Science (New York, N.Y.),123(3191), 309-314. doi: 10.1126/science.123.3191.30
Wheless, J. W. (2008). History of the ketogenic diet. Epilepsia, 49(8), 3-5. doi: 10.1111/j.1528-1167.2008.01821.x
Wilder R. M. (1921). The effect of ketonemia on the course of epilepsy. Mayo Clinic Bulletin. 2: 307.
Woodyatt R. T. 1921.Objects and method of diet adjustment in diabetics.Archives of Internal Medicine,28(2). doi: 10.1001/archinte.1921.00100140002001