The Use of Tryptophan to Treat Depression
/By: Elika Imandel
As the leading cause of disability worldwide, depression affects more than 300 million people (Depression, 2018). Major Depressive Disorder (MDD) is a mental disorder of complex etiology. Depressed mood and loss of interest in daily activities are core features of a major depressive episode (Kennedy, 2008). Synthesized with the amino acid tryptophan, the neurotransmitter serotonin is involved in mood regulation; specifically, decreased levels have been shown to contribute to an increase in symptoms of depression (Lindseth, Helland, & Caspers, 2015). In an attempt to challenge the status quo, current interventions for MDD must be explored, identifying the specific effects neurotransmitters have on depression, and determining how tryptophan could potentially be used to treat depression.
An early theory of depression was the monoamine hypothesis. The monoamine hypothesis suggests that the underlying pathophysiological cause of depression is due to depleted levels of the monoamine neurotransmitters norepinephrine (NE), serotonin, and/or dopamine (DA) in the central nervous system (Delgado, 2000). Today, there are far more theories about the cause of depression, one theory hypothesizes that diminished levels of serotonin in the brain play a role in the pathophysiology of depression (Cowen & Browning, 2015). Current treatments for depression include antidepressants such as selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), and norepinephrine-dopamine reuptake inhibitors (NDRIs). Those suffering from depression have depleted levels of serotonin, and SSRIs are the most common drug prescribed for treatment (Depression: How Effective are Antidepressants, 2017). SSRIs block the reuptake of serotonin into the presynaptic neuron, thus allowing for an increase in availability between neurons in the synaptic space. Consequently, by allowing serotonin to remain in the synaptic space for a longer period of time, the excess serotonin has an opportunity to recurrently stimulate the postsynaptic receptors; thus, mirroring the response of a healthy neuron. Although further research is required, manipulation of tryptophan, a precursor to serotonin in the brain, via supplementation may be an alternative to medication in alleviating depression or symptoms of depressed mood.
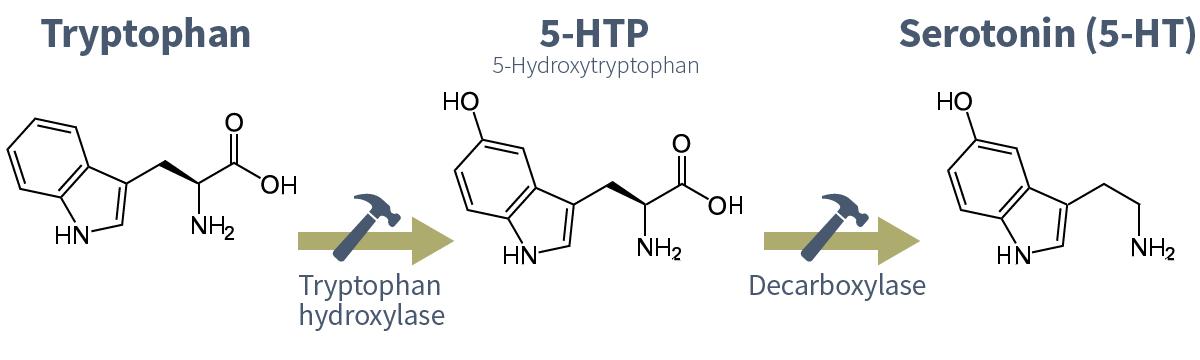
Being the precursor for the production of serotonin, tryptophan also plays a role in mood regulation. With its overall concentration being the lowest among all amino acids, tryptophan has comparatively low tissue storage in humans (Richard et al., 2009). Tryptophan can be found in various foods, such as meats, fruits, and dairy. Upon consumption, tryptophan is distributed throughout the body. Its high affinity for the blood-brain barrier (BBB) transporter allows for it to be taken up into the brain. In the brain, tryptophan is first converted into 5-hydroxytryptophan (5-HTP) by the tryptophan hydroxylase enzyme; the activity of this enzyme is dependent on the availability of tryptophan in the brain (Richard et al., 2009). Finally, 5-HTP is converted into serotonin via the aromatic amino acid decarboxylase enzyme. Foods with a high glycemic index, meaning they quickly increase blood glucose levels, have been shown to increase the availability of tryptophan (Jenkins, Nguyen, Polglaze, & Bertrand, 2016). Upon ingestion of carbohydrates, many of which have a high glycemic index, insulin drives selective amino acids into muscle tissue. Tryptophan, which normally competes with the branch-chained amino acids Leucine, Isoleucine, Proline, and Valine in plasma, is then able to cross the BBB more freely (Jenkins et al., 2016). Thus, the level of tryptophan in the brain is increased, facilitating an increase in serotonin production. This increase in serotonin levels allows for a rise in one’s overall mood and happiness.
Current research has shown that certain foods high in tryptophan have the potential to decrease anxiety and depression. Interestingly, in a three-week randomized crossover clinical trial conducted by “Badrasawi, Shahar, Manaf, and Haron (2013) 30 depressed elderly individuals (9 women and 21 men) were given Talbinah, a Malaysian food that is high in carbohydrates and tryptophan. One group was served Talbinah daily, while the control group was not; the candidates were assessed in weeks 0, 3, 4, and 7. Upon concluding the study, it was found that those given Talbinah had reduced levels of depression and stress with an overall increase in their mood. The results of this study substantiate the claim that increased levels of serotonin reduce levels of stress and depression.
In another tryptophan supplementation study, conducted by Lindseth et al. (2015), 25 participants were randomly given two, 4-day dietary treatments. One group was given a diet with > 10 mg/kg body weight of tryptophan per day and the other was given a diet with < 5 mg/kg body weight of tryptophan per day. The results indicated that the participants given > 10 mg/kg body weight per day had significantly less depression when compared to those consuming < 5 mg/kg body weight. Thus, as supported in the previous claim, increased levels of dietary tryptophan per day further reduce levels of stress and depression.
Although existing results are limited, these studies show tryptophan supplementation has potential as a treatment for depression. The amino acid tryptophan is a precursor for the synthesis of serotonin. It is hypothesized that diminished levels of serotonin in the brain plays a role in the pathophysiology of depression (Cowen & Browning, 2015). Further study is essential to better understand how tryptophan supplementation can best be used as an alternative to current medications to combat depression. With an increase in those affected by depression, it is important to look for alternative forms of treatment, like food, rather than medication which can create a society reliant on prescription drugs.
References
Badrasawi, M. M., Shahar, S., Manaf, Z. A, & Haron, H. (2013). Effect of Talbinah food consumption on depressive symptoms among elderly individuals in long term care facilities, randomized clinical trial. Clinical Interventions In Aging, 8, 279. doi: 10.2147/cia.s37586
Cowen, P. J., & Browning, M. (2015). What has serotonin to do with depression? World Psychiatry, 14(2), 158–160. http://doi.org/10.1002/wps.20229 Depression. (2018). Retrieved from http://www.who.int/news-room/fact-sheets/detail/depression
Delgado, P. (2000). Depression: The case for a monoamine deficiency. Retrieved from http://www.psychiatrist.com/jcp/article/pages/2000/v61s06/v61s0603.aspx
Jenkins, T. A., Nguyen, J. C. D., Polglaze, K. E., & Bertrand, P. P. (2016). Influence of Tryptophan and serotonin on mood and cognition with a possible role of the gut-brain axis. Nutrients, 8(1), 56. http://doi.org/10.3390/nu8010056
Kennedy, S. H. (2008). Core symptoms of major depressive disorder: Relevance to diagnosis and treatment. Dialogues in Clinical Neuroscience, 10(3), 271–277.
Lindseth, G., Helland, B., & Caspers, J. (2015). The effects of dietary tryptophan on affective disorders. Archives of Psychiatric Nursing, 29(2), 102–107. http://doi.org/10.1016/j.apnu.2014.11.008
Richard, D. M., Dawes, M. A., Mathias, C. W., Acheson, A., Hill-Kapturczak, N., & Dougherty, D. M. (2009). L-Tryptophan: Basic metabolic functions, behavioral research and therapeutic indications. International journal of tryptophan research: IJTR, 2, 45–60.